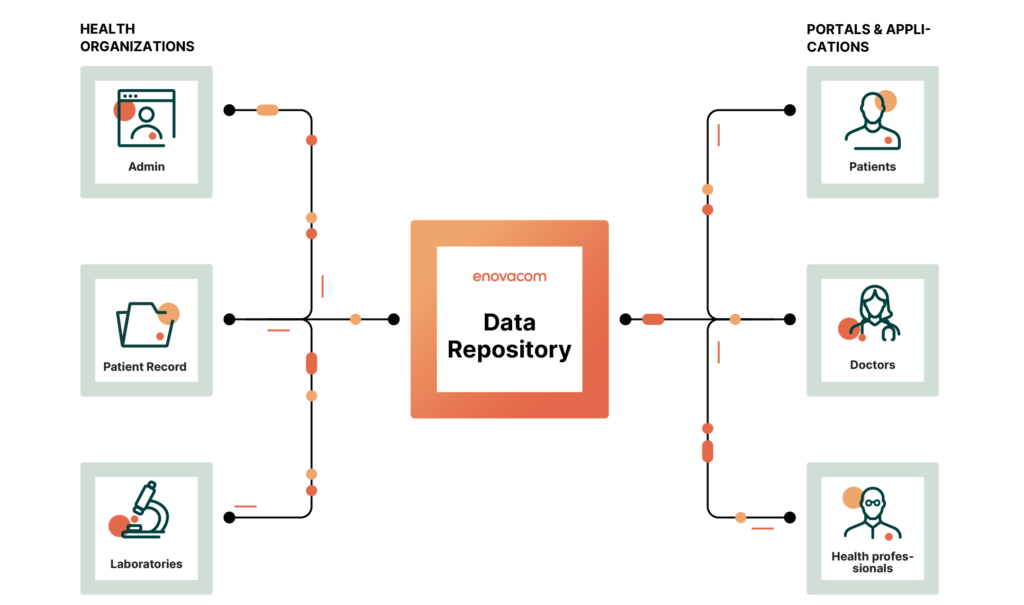
A FHIR data warehouse to enhance your data from a single storage space and make data sharing and access easier.
Why choose Enovacom's FHIR data warehouse?
Collaboration
Create a link between the professionals and organizations involved in a patient’s care by sharing data in an accessible way.
Enhancement
Re-use and enrich the data in your warehouse so that the information can be used beyond a simple exchange.
Interconnection
Simplify data exchange between information system applications and your vendor-neutral data warehouse, ensuring everything is transparent.
- Data is stored in accordance with the FHIR standard.
- The customer chooses the FHIR version.
- Profile integration.
- Direct connection or via the Enovacom Integration Engine.
- Development of personalised portals.
- Data stored in a shared space.
- Departmentalised data.
- Data enriched by connecting multiple sources.
- Development of innovative projects with your data.
Technical platform
- Web application.
- FHIR.
- Relational and non-relational databases.
- Linux environments, physical or virtual servers.
Compatibility with Microsoft 365
The data repository is designed to aid the exchange and sharing of medical information about the patient. This is why Enovacom has developed a project to integrate its repository with Microsoft. The Cloud Suite of Microsoft 365, as well as its Azure Active Directory, are compatible with Enovacom Data Repository.
What our customers say about Enovacom's FHIR data warehouse
Our institutions are adopting a digital strategy based on the FHIR standard, and Enovacom’s data warehouse was the most mature solution to address this challenge.
Pascal CousinCIO, Cliniques de l'Europe, Belgium 
We can now store all our sample data from our biobanks in an interoperable data warehouse, enabling us to list and reuse our samples.
Pr. Pierre-Edouard FournierDirector of IHU Mediterranée Infection, France 
